Background: Oxbryta is a recently approved drug for patients with Sickle Cell Disease (SCD), which decreases HbS polymerization, thus reducing red cell hemolysis and increasing hemoglobin concentration. It was first available for Expanded Access May 9, 2019 and received fast track approval for commercial use by the FDA on November 25, 2019.
Objective: This analysis aims to gain insights to the real word experience for patients with SCD who are prescribed Oxbryta, identify barriers to its use, and measure health outcomes.
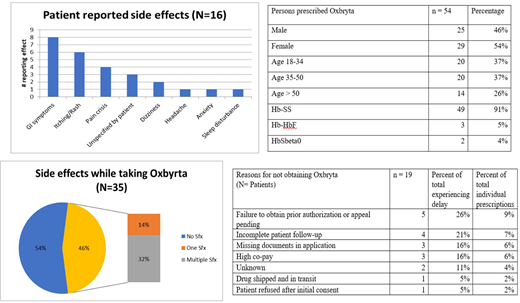
Methods: Electronic medical records of 54 patients with SCD who were prescribed Oxbryta from January until June 2020 were reviewed and evaluated for data regarding demographics, initiation of treatment, hematological response, side effects, dosage modifications and terminal discontinuations.
Results: A total of 54 patients were prescribed Oxbryta in the study period who were 96% (52/54) HbSS, and 4% HbSβ0 (2/54); 46% (25/54) male and 54% (29/54) female, and a mean age of 41 years (range 21-70). At time of initiation, 52% (28/54) of patients were taking hydroxyurea (HU). Indication for initiation of therapy was anemia and hemolysis. In this cohort, 65% of patients (35/54) were able to access drug with a mean time to obtain drug of 45 days (range 0-118 days). The most common barriers to obtaining drug were: requiring a prior authorization or appeal 9% (5/54), incomplete patient follow up 7% (4/54), missing documentation for application 6% (3/54) and high patient co-pay 6% (3/54). Of the 35 patients who started Oxbryta, 46% (16/35) experienced at least 1 side effect with 31% (11/35) reporting multiple side effects. The most common side effects reported were gastrointestinal distress (abdominal pain, nausea, vomiting and/or diarrhea) in 23% (8/35), dermatologic effects (itching and/or rash) in 17% (6/35), and experiencing an acute VOC or increase in daily pain in 11% (4/35). Twenty nine percent (10/35) of patients required a dose modification to address side effects (half who successfully continued the drug on a modified dosage), an additional 23% (8/35) of patients terminated usage of Oxbryta in response to side effects. After two to four weeks of taking Oxbryta 63% of patients had a hemoglobin increase of at least 1g/dl or greater.
Conclusion: Oxbryta produces a substantial rise in hemoglobin for persons living with sickle cell and high baseline levels of hemolysis in about 60 % of patients, similarly to the results from the HOPE trial. However, there are significant barriers to access that require close follow up in the immediate period following prescription of the drug in order to minimize delays in access. Furthermore, in our cohort we observed a higher incidence of side effects than the 23% (900mg) -26% (1500mg) reported in the pivotal trial that led to its approval. While some individuals were able to be continue therapy after dose modifications, most discontinued therapy because of side effects.
Minniti:CLS Behring: Consultancy; Roche: Consultancy; Emmaus: Consultancy; Forma: Consultancy; Global Blood Therapeutics: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees; Teutona: Membership on an entity's Board of Directors or advisory committees; Bluebird Bio: Other; Sodium Nitrate for SCD leg ulcers: Patents & Royalties.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal